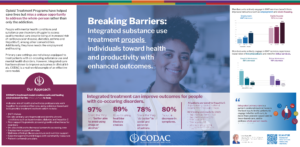
Poster presented at 2024 RxSummit
Download Poster PDF
Presenter Bio
Larry Onate, MD, Medical Director of Addiction Services
 Larry Onate, MD is the Medical Director for CODAC’s Addiction Services programs. He completed both his undergraduate and medical degrees in Arizona. He completed his Internship at the University of California San Francisco. Dr. Onate went on to complete his residency in psychiatry at the University of Arizona in 1993. He was awarded the American Academy of Child and Adolescent Psychiatry Charter Fellowship in 1991.
Larry Onate, MD is the Medical Director for CODAC’s Addiction Services programs. He completed both his undergraduate and medical degrees in Arizona. He completed his Internship at the University of California San Francisco. Dr. Onate went on to complete his residency in psychiatry at the University of Arizona in 1993. He was awarded the American Academy of Child and Adolescent Psychiatry Charter Fellowship in 1991.
Dr. Onate’s work experience includes serving as Medical Director at the following agencies:
Cottonwood de Tucson, 2010-2017; Southern Arizona Mental Health Corporation Crisis Center,
2000-2010; La Frontera, Inc., 1996-2000; and Desert Hills Center for Family and Youth-
Adolescent Inpatient Unit, 1993-1996. Dr. Onate has served as Medical Director of CODAC’s Addiction Services since 2017.
Expanding Upon the Information in the Poster
Opioid Treatment Programs (OTPs) have historically addressed opioid dependence in individuals. While this focus has saved lives and helped spur recovery, it misses a unique opportunity to address the person rather than just the addiction. Health issues as a whole are common in the individuals served through OTPs including an increasing prevalence of Hepatitis C virus infections along with HIV, other sexually transmitted infections, COPD, diabetes, hypertension and other cardiac and health issues related to opioid use.
At the CODAC Health, Recovery & Wellness clinic in Tucson, Arizona, injection point infections were among the leading causes of hospitalization and rehospitalization of individuals in opioid treatment. All these disparate health issues spurred the original drive toward integrated whole-person care in the OTP.
By removing barriers to care found in the traditional healthcare silos and seeing clients/patients as a whole person, not just an addiction, and focusing on all dimensions of wellness, especially health concerns, stronger patient-centered relationships can be forged. Additionally, greater participation in services helps address a wider variety of needs including health care, employment services, housing, identification cards, transportation, employment opportunities and other social determinant needs.
The traditional OTP treats opioid dependence. For any other needs identified, referrals are made to community providers. Given the extent of co-occurring health issues and social determinant needs within this population, a different model may be indicated.
Integrated multidisciplinary care models can better engage and retain individuals. This is seen as critical to the success of HIV and HCV prevention strategies. Key components such as provision of MAT, HIV and HCV treatment to prevent transmission, access to HIV pre-exposure prophylaxis, and behavioral health services that address psychiatric co-morbidities will increase engagement with and adherence to care (Rich, Bia, Altice and Feinberg 2018).
Patients who are actively engaged in therapy for addiction have a better opportunity to identify diseases and chronic conditions such as HCV or HIV. Yet most patients undergoing methadone maintenance treatment (MMT) are never screened for Hepatitis C virus (HCV) infection. And for those that are diagnosed, a gap exists between the OTP and the HCV provider as fewer than one third of people referred receive follow-up care at the HCV clinic (Chi-Ming Tai et al, 2019).
The importance of the multidisciplinary team composed of medical, addiction medicine, psychiatrists and other providers of social needs is demonstrated through engagement and successful attainment of multiple goals including on-going treatment of chronic issues such as diabetes and HIV, identification and intervention for cardiac issues, HCV, injection point infections highlight the potential if addiction treatment is separate from primary care and other providers (Tunyan, Hewitt, Martin, & Mullin 2017).
Opioid use disorder and other substance use disorders have an impact across multiple disciplines. Historically, care is siloed with different providers, each looking at a part of the person and not the whole person. Yet individuals diagnosed with substance use disorders also have myriad medical needs, other mental health issues as well as additional social needs like employment and housing needs. Many times, referring to integrated care refers to addiction and mental health being treated either through co-location or integration even as research is showing that ALL needs of an individual are best addressed through integration or co-location. AT CODAC, we have found that integrated whole person care is best provided in a behavioral health/substance use disorder setting with PCP services integrated into the practice. This is because the behavioral health/substance use disorder setting is best equipped to deal with issues and behaviors that a prominent in this setting, especially upon initiating treatment with the target population. Safety in this environment is paramount for recovery, health promotion and staff safety and retention.